CKD PATIENT CASE 2
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box"
Chief complaints
History of present illness
Daily routine
Wakes up at 6am
breakfast - 7.30
Goes to factory- 8am
1pm - lunch
4.30pm- tea
6pm - home
8pm - dinner
Alcohol- 2 times a week, 180 ml. Since past 15 years
Past history
Family history
Personal history
Family history
General examination
Patient is conscious, coherent and co-operative.
Examined in a well lit room.
Moderately built and nourished
Vitals :
Temperature- afebrile
Respiratory rate - 28 cpm
Pulse rate - 76 bpm
BP - 120/80 mm Hg.
Spo2 at room air is 98%
SYSTEMIC EXAMINATION:
CVS : S1 S2 heard, no murmurs
Respiratory system : normal vesicular breath sounds heard.
Abdominal examination:
INSPECTION :
Shape of abdomen- distended
-No tenderness of abdomen
- Umblicus - normal
- Movements of abdominal wall - moves with respiration
- Skin is smooth and shiny;
- No scars, sinuses, distended veins, striae
PALPATION :
No Local rise of temperature
Tenderness absent
Guarding present
Rigidity absent
hernial orifices normal
Fluid thrill absent
Liver not palpable .
Spleen not palpable
Kidneys not palpable
Lymph nodes not palpable
PV examination -normal
P/R examination -normal
.
CNS EXAMINATION:
Conscious
Speech normal
No signs of meningeal irritation
Cranial nerves: normal
Sensory system: normal
Motor system: normal
Reflexes: Right. Left.
Biceps. ++. ++
Triceps. ++. ++
Supinator ++. ++
Knee. ++. ++
Ankle ++. ++
Gait: normal
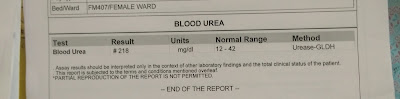
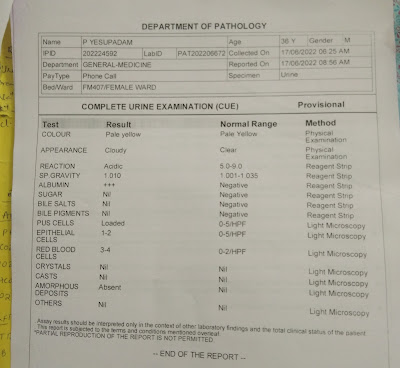
Investigations
Serology:
HIV - negative
HCV - negative
HBsAg - negative

















Comments
Post a Comment